The Future of Vaccines Achilles Gravanis
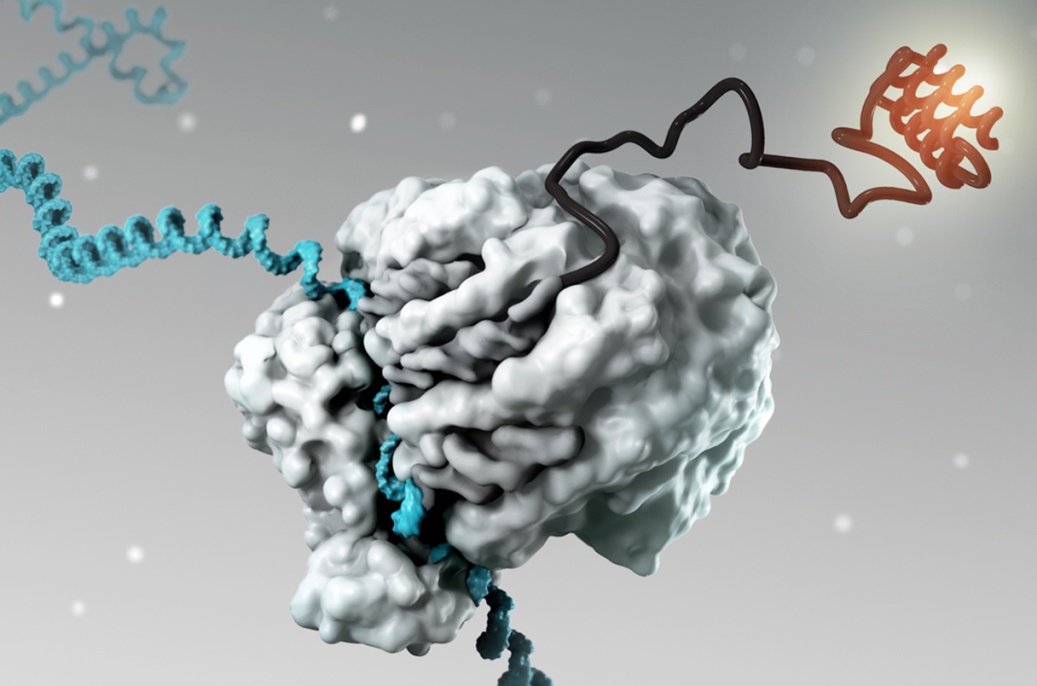
Messenger RNA, or mRNA, was discovered in the early 1960s, while in the 1970s research was developed on how it could be administered to cells and later as medicine. The biggest challenge has been how mRNA could be administered to the body since is quickly rebuilt, before it can “deliver” its message – the RNA transcript – to be read, converted into pharmacologically active proteins in cells. The solution to this problem came from the progression of nanotechnology and the development of fat droplets (lipid nanoparticles) that “wrapped” the mRNA like a bubble and protected it, that allowed it to enter the cells. Furthermore, changing a single nucleoside component with another artificial one gave the mRNA enough stability to allow it to enter the cell. The first mRNA vaccines using these “fatty bubbles” were developed against the deadly Ebola virus but, since this virus is only found in a limited number of African countries, they have not been developed in the rest of the world. The development of mRNA vaccines is, however, is the total evidence of the extraordinary importance of basic biomedical research, the findings of which usually become clinically useful years later at an unsuspected time, as in the case of the 2020 coronavirus pandemic.
The first combined mRNAs vaccine arrive
The spread of other epidemic respiratory diseases during the cold season increases the risk of co-infections with two or more respiratory pathogens. One of the most common respiratory pathogens is the influenza virus, which has been reported to co-infect with the coronavirus. Several recent studies have suggested that influenza virus infection facilitates the entry of the coronavirus into host cells, subsequently leading to severe pneumonia and lung damage. Thus arose the urgent need to develop a combination vaccine capable of providing protection against both coronavirus and influenza at the same time. A recent study, one of many already underway, highlighted the efficacy of an mRNA vaccine referred to as ARIAV, which encodes the hemagglutinin (HA) antigen of the H1N1 influenza virus. The ARIAV vaccine was integrated into a previous mRNA vaccine ( ARCoV ) encoding the binding region of the coronavirus to its cellular receptor to yield a combined vaccine formulation referred to as AR-CoV/IAV. This study, like others, showed that a combined mRNA vaccine is capable of inducing broad and durable protection against co-infection with multiple variants of coronavirus and H1N1 influenza virus. It is very possible that in the next few years, perhaps even in 2025, we will have the first combined mRNA vaccines against the influenza viruses and the coronavirus, in one administration. After Ebola and the coronavirus, mRNA vaccine technology is now being extended to other infectious diseases, such as those from the Zika and Chikyngunya viruses, the parainfluenza virus PIVR, cytomegalovirus (CMV), rabies virus (Rabies lyssavirus), the respiratory syncytial virus (RSV), the human papillomavirus (HPV) and also the HIV virus of AIDS. Pharmaceutical companies such as Moderna, GSK, Merck, Curevac relevant phase ½ clinical studies are already underway. In the two years 2023-24 there will be new MRNA vaccines against some of the above infectious diseases in the prescription.
Intranasal vaccines are coming
In the case of the coronavirus pandemic, currently used vaccines are highly effective at reducing disease severity and preventing hospitalization, but not as well at preventing mild disease or its transmission. Administering them intramuscularly triggers an immune response that includes T-lymphocytes, which destroy infected cells, and B-cells, which produce antibodies that neutralize the virus, binding it and preventing it from entering healthy cells. These immune cells and antibodies circulate in the blood but do not end up in high enough numbers in the nose and lungs to provide full protection. In the time it takes for them to collect there from the bloodstream, the virus spreads and the person becomes ill. In contrast, mucosal vaccines can induce a whole-body immune response but can also activate immune cells in the mucosal tissue of the nose and respiratory tract. These localized cells act as sentinels at the point of entry of infection thereby preventing not only severe disease but also transmission of the virus. Localized mucosal immune cells, known as tissue-resident memory T and B cells, have slightly different functions than circulating blood T and B cells. For example, tissue-resident memory B cells produce antibodies of the secretory immunoglobulin A (IgA) type, which are able to quickly stop the virus before it infects the body. More than 100 intranasal vaccines are being developed worldwide. The first attempts were not successful because the vaccine did not stay long enough in the nose; it went down into the stomach and was destroyed. New pharmaceutical forms are expected that will keep them in the nose for a sufficient time for an immuno-effective immunization. Intranasal vaccines will change the picture of Corona infection by drastically limiting its transmission in the community. They are expected within the next one to two years.
Applications to other diseases
Nucleic acid vaccine technology, such as mRNA and Cdna-vector vaccines, is now finding applications in diseases other than infectious ones. Indeed, cDNA-vector vaccines are being developed against diseases such as cancer and neurodegenerative diseases. Therapeutic cDNA-vector vaccines are already being tested in patients with breast, prostate, lung, pancreatic and melanoma cancer, with very encouraging first clinical result. The related vaccines target tumor associated antigens (tumor associated antigens or neoantigens) as well as tumor cytokines, offering new therapeutic weapons in cancer immunotherapy, apart from these cell therapies (CAR T-cells). The first therapeutic vaccines against cancer are expected within the next one to two years. Also, experimental mRNA vaccines have already been developed against multiple sclerosis and Alzheimer’s disease, focusing on their pathological factors such as the proteins myelin, tau, a-synuclein, etc.
Mr. Achilleas Gravanis is Professor of Pharmacology at the School of Medicine of the University of Crete, IMBB-FOTH researcher and Associate Research Professor at the Center for Drug Development at Northeastern University (Boston).
SOURCE: To Vima newspaper 4-12-2022
Translation editor: Dr. Eleni Paximadi
I am especially happy because I was asked kindly from a friend to translate from Greek to English